ARFID Kids Camp- Initial Deposit
Join our comprehensive 8-hour program, featuring 2 hours of daily activities focused on food exploration and education tailored specifically for children with ARFID sensory-sensitivity type. Our program incorporates evidence-based treatments for ARFID including FBI-ARFID, responsive feeding, and CBT-AR techniques. This program aims to empower kids to explore new foods, increase their awareness of their sensory …
![Eating on a date with ARFID [Image description: a man and a woman smiling at each other seated at a table. The man holds a glass and the woman has food in front of her] Depicts a potential couple on a date where one of the members has ARFID](https://www.eatingdisordertherapyla.com/wp-content/uploads/2025/02/happy-valentines-day-1807617_1280-1024x682.jpg)
![ARFID and Holidays [Image description: Purple scrabble tiles spelling "ARFID and Holidays"]](https://www.eatingdisordertherapyla.com/wp-content/uploads/2024/11/IMG_3940-1024x718.jpg)
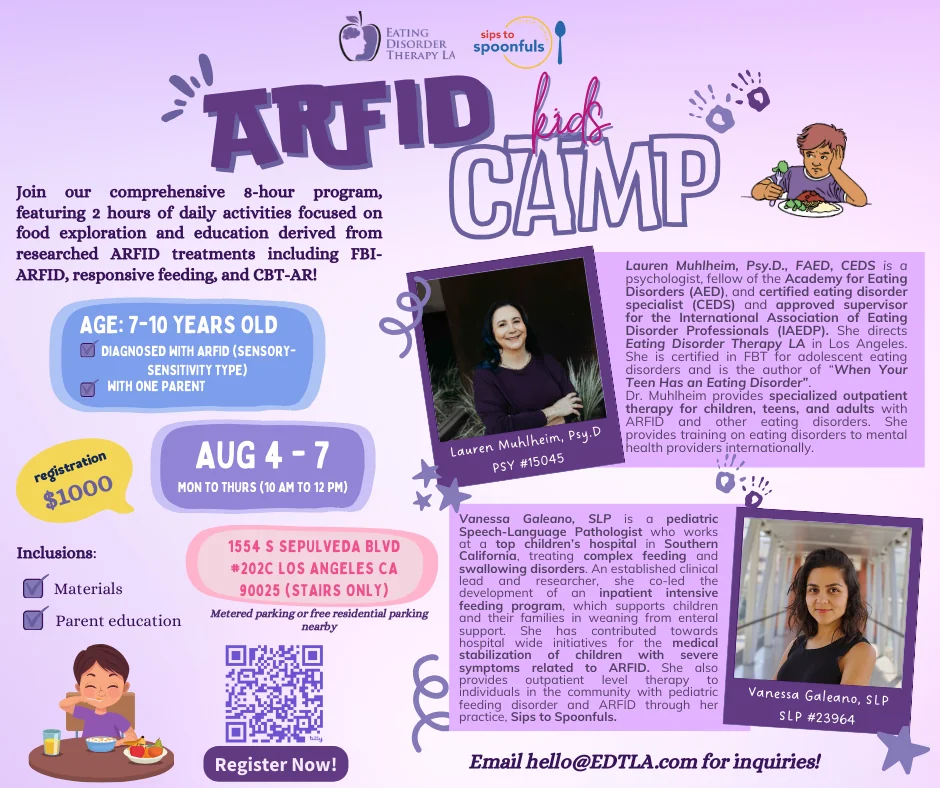
![ARFID Kids Camp 2025 [Image description: details also in text below for ARFID camp 2025 for kids 7 to 10]](https://www.eatingdisordertherapyla.com/wp-content/uploads/2024/05/ARFID-CAMP-2025_updated-FB-Post.png)
![Supporting a friend with ARFID in California [Image description: a woman with her hand on the shoulder of another woman who appears distressed] Represents a potential client getting help for ARFID in California](https://www.eatingdisordertherapyla.com/wp-content/uploads/2023/09/pexels-liza-summer-63831581-1024x682.jpg)
![Feeding a Child with ARFID in Los Angeles, California [Image description: photo of a girl eating broccoli and rice and looking unhappy] Represents a child with ARFID in therapy in California](https://www.eatingdisordertherapyla.com/wp-content/uploads/2023/07/686112772-huge2-1024x683.jpg)
![Therapy for ARFID in Children in California [Image description: a boy eating breakfast of cereal and juice and looking unhappy] Represents a potential client receiving counseling for ARFID in California](https://www.eatingdisordertherapyla.com/wp-content/uploads/2023/05/Shutterstock_10970257732-1024x683.jpg)
![Helping Others in Your Life Understand Your ARFID [Image description: 4 friends of diverse sizes and skin colors sitting at a picnic table] Represents supportive friends of a potential client seeking help for ARFID in Los Angeles, CA](https://www.eatingdisordertherapyla.com/wp-content/uploads/2023/04/allgo-an-app-for-plus-size-people-1qS6wnebTsM-unsplash1-3111-21-1024x683.jpg)
![Adults with ARFID in Los Angeles, California [Image description: drawing of a woman looking at her food and eating very slowly] Represents a potential adult patient with ARFID seeking counseling in Los Angeles, California](https://www.eatingdisordertherapyla.com/wp-content/uploads/2022/10/My-project14.png)
![ARFID and Diet Culture in Los Angeles, California [Image desciption: photo of a woman buying bread] Represents a potential eating disorder client in Los Angeles, California standing up to diet culture](https://www.eatingdisordertherapyla.com/wp-content/uploads/2022/08/pexels-uriel-mont-62803981-1024x683.jpg)