TL;DR
Early intervention is crucial in addressing eating disorders, which can lead to severe health issues if not treated promptly. Family-Based Treatment (FBT) is a leading, evidence-based approach tailored for teens, emphasizing parental involvement to support recovery. Despite its potential benefits, parents often hesitate to intervene due to uncertainty about the early signs of these disorders.
Both case studies outlined in this blog underline the importance of early intervention using FBT, which can prevent the escalation of eating disorders. Parents are encouraged to recognize early signs and engage in supportive strategies, as timely action can lead to healthier outcomes for their children. If you’re seeking early intervention support through FBT in Los Angeles, consider reaching out for guidance and assistance.
Does FBT Help Parents With Early Intervention For Eating Disorders?
Originally published on the F.E.A.S.T Blog on August 22, 2014, by Lauren Muhlheim, Psy.D., CEDS, and Therese Waterhous, PhD/RDN
Eating Disorders are serious mental illnesses with dangerous medical consequences. Without early intervention, eating disorders may become chronic or even fatal. Parents are often unaware of some of the early signs of an eating disorder. Even if they are aware of early warning signs, they are often uncertain and reluctant to intervene out of fear of worsening the situation.
Family-Based Treatment (FBT) is one of the leading evidence-based treatments for teens with eating disorders. Although not well-studied as an early intervention, one small study found that family-based early intervention for anorexia nervosa in teens is feasible and potentially beneficial.
Below, we describe how two clinicians trained in the provision of FBT applied FBT principles to help their children who showed some very early warning signs of an eating disorder.
What are the Challenges of Early Eating Disorder Intervention?
 Eating disorders are notoriously hard to spot in the early phases. In the movie, Spotting the Tiger: Recognizing Early Signs of Anorexia in Children, narrated by Jamie Lee Curtis, she states, “Recognizing anorexia early is like trying to spot a tiger in the jungle. Trackers will tell you they never see the tiger, only the evidence of where it’s been. If you actually see the tiger, you are already in danger. The same is true of anorexia. When anorexia is obvious, serious damage has already been done.”
Eating disorders are notoriously hard to spot in the early phases. In the movie, Spotting the Tiger: Recognizing Early Signs of Anorexia in Children, narrated by Jamie Lee Curtis, she states, “Recognizing anorexia early is like trying to spot a tiger in the jungle. Trackers will tell you they never see the tiger, only the evidence of where it’s been. If you actually see the tiger, you are already in danger. The same is true of anorexia. When anorexia is obvious, serious damage has already been done.”
Once an eating disorder has fully developed, parents usually look back with regret; they often identify numerous early warning signs that they missed. Because the signs are generally so subtle and, in many cases, look innocuous or even “healthy,” most parents are not prepared to intervene. Even pediatricians commonly advise parents to “watch and see what happens” before intervening. However, the development of an eating disorder is a slippery slope, and the situation can rapidly progress from mild to severe.
What are Potential Eating Disorder Warning Signs in Children and Teens?
- Any weight loss in a growing child (even if the child was initially overweight). NOTE: Teens may lose weight for a variety of reasons; rule out other causes such as type 1 diabetes
- Dieting behavior or intention
- Rejection of foods or food groups previously enjoyed by a child or teen
- The child or teen skipping meals or saying they have already eaten
- Increased physical activity or movement (may not be goal-directed) in a teen or preteen not accompanied by increases in food consumption
- Failure to gain weight in a growing child or teen
- Slowing of the rate of gains in height
- Preoccupation with food preparation, recipes, or cooking shows
Children and Adolescents Who May Be At Increased Risk
Although we do not understand all of the risk factors for developing an eating disorder, the following are some factors that may increase an individual’s risk for developing one.
- Family history of anxiety-related disorders
- First-degree relative with a diagnosis of an eating disorder
- Traits of perfectionism
- History of anxiety
How Can Parents Use FBT Strategies For Early Intervention?
Below are two case studies of how FBT-trained clinician parents used Family-Based Treatment for an early intervention.
Case 1: Alexandra
“Alexandra” is the middle of three children, female, age 11.5 at the time of the intervention. She has always been very active. Alexandra has always been a picky eater, especially about textural issues; for example, she has never liked crusts on bread, fat on meat, fried food, or potatoes. She is perfectionistic and competitive. She has tracked around the 50th percentile in weight for most of her childhood, slightly higher in height.
Specific warning signs and indicators for intervention:
- Over the previous two years, Alexandra’s weight percentile had been slowly declining (from the 35th percentile down) while her height percentile was constant at 50%.
- Alexandra became extremely interested in food preparation, cooking, reading recipes, and watching cooking shows.
- Alexandra’s family moved home from an international assignment (a major stressor)
- Alexandra’s physical activity increased significantly as she progressed from recreation soccer to club soccer (the commitment increased from 2 days per week to 6 days per week). At the same time, her appetite and food consumption did not, on their own, increase.
- She did not ask for more food, but she also never expressed any dieting concerns or any concerns about shape or weight.
- On a day off from school, Alexandra ran 2.5 miles, then stated she “felt great” immediately afterward. Following the run, she refused a meal of eggs (food she has never liked) and bacon (she proceeded to pick the fat off the turkey bacon because of complaints about the texture). She was content to eat nothing when she didn’t like the options available.
- However, she would eat foods such as desserts when offered
Parental interventions:
Parents agreed to do FBT early intervention with a focus on parents observing her eating during meals and helping her to eat enough to fuel for increased physical activity and growth.
Alexandra’s soccer practice was often during dinner, and she would often come home tired and uninterested in dinner. Alexandra’s parents structured her meals, requiring her to eat before soccer practice. If her parents did not feel she had eaten enough, they would coach and insist.
In the few situations where there was a predominance of foods she may never have eaten (due to the textural issue), parents offered alternatives to ensure she ate enough (distinct from the strategy parents used with the other children, which was offering no alternatives to the primary meal in an effort to promote eating flexibility). Parents instituted regular weighings and spoke to her about their concerns.
Results
Over a four-month period during the intervention, Alexandra gained 6 pounds even as she joined a club soccer team and increased her physical activity. Eventually, her appetite did seem to “catch up” to her need, and her parents gradually reduced their oversight. The parents believe they helped Alexandra to keep up with her increased energy needs during this critical time period when she appeared unable–at least initially–to do so on her own. Anorexia nervosa can appear insidiously in situations like this (independent of any intention to diet or lose weight), so this early parental intervention is believed to have been effective based on FBT principles.
Over a two-year period, Alexandra gained about 18 pounds while growing 6.5 inches. Menarche occurred at age 13.5. At age 15, she is now fully back on her growth curve with height at the 75th percentile and weight at the 50th percentile. She eats normally and intuitively. It is notable that she no longer has a strong interest in cooking and cooking shows.
Case 2: Jack
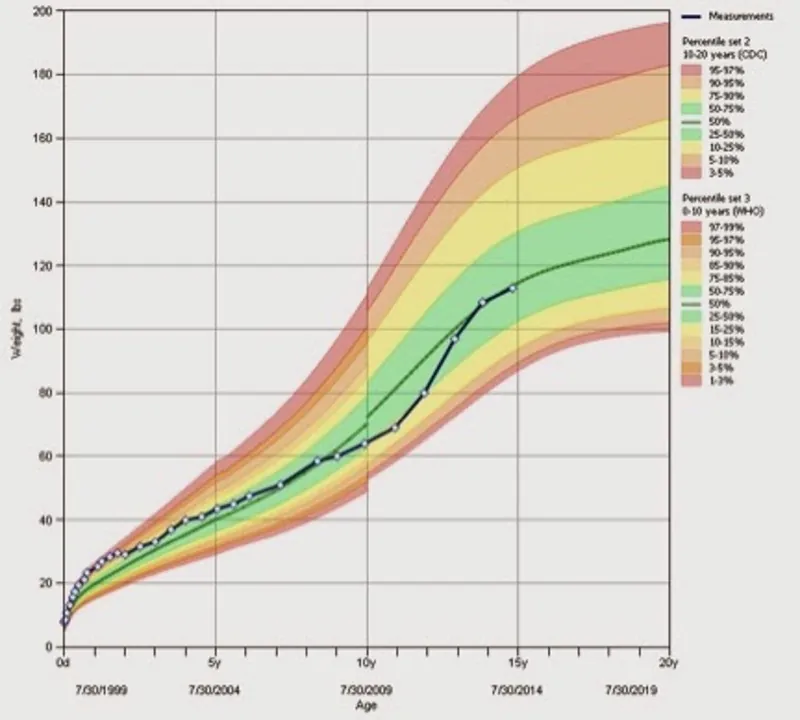
“Jack” is a 15-year-old high school freshman who, at age 9 months, showed some early signs of food selectivity and avoidance of certain tastes and textures. He has never shown a large growth spurt but rather tracked along the same percentiles for much of his life. According to his parents, Jack has been a typical “kid eater,” preferring easy, bland, non-mixed foods and demonstrating food neophobia, typical in many toddlers and young children.
Growth charts show that from age 1 year until age 15, he was atthe 5th percentile for height and 10th to 25th for weight. Growth has been consistent, but the child’s pediatrician did order growth hormone levels measured, which showed a normal level of growth hormone. Jack was competitive but not overly perfectionistic, yet as Jack started high school, he stated he wanted to achieve all A’s for all years of high school. His body type is muscular.
Specific Warning signs and indicators for intervention:
- During the previous year, Jack significantly increased physical activity, participated in soccer conditioning camps, played JV soccer for high school, and recently joined a soccer club.
- Jack was not particularly interested in increasing food intake, nor did he show a greatly increased appetite.
- After 1 week of soccer conditioning, he showed a weight loss of 6 pounds.
- Jack has a full sibling diagnosed with anorexia nervosa at age 13, now recovered.
Parental intervention
Parents agreed to intervene by increasing caloric intake appropriately, taking weekly weighings, and providing guidance about the need to fuel increased exercise and hydrate for intense activity. His parents ensured he consumed all meals and adjusted schedules accordingly to allow for snacks to be made and eaten before or after school and soccer activities. He was not allowed to miss meals and snacks.

Jack did complain of feeling overly full on several occasions, and his parents did not give in to the desire to allow decreased food intake. Parents increased his caloric intake by adding oils to foods such as pasta and rice, adding Instant Breakfast to milk, increasing portion sizes of meals, and requiring 2 snacks per day, minimum.
Results
Jack restored weight within 2 weeks. Weight monitoring continued through the freshman year of high school to ensure that Jack met the expected gains in weight and height. Over time, he maintained his weight and grew as expected according to lifetime growth charts. Gradually, he was given more freedom to portion his food, choose snacks, and have flexibility in terms of the timing of snacks. Breakfast, lunch, and dinner were usually prepared and served family-style. Jack usually chose and prepared his snacks, a developmentally appropriate option when no eating disorder is present.
Two years later, Jack has continued to develop normally, gaining expected height and weight. He eats a wider variety of foods and is less concerned about textures and new tastes. Given the positive family history of anorexia nervosa, it is especially appropriate to catch weight loss in a growing sibling early. Weight loss, whether intentional or not, is a significant trigger for the initiation of eating disorder pathology.
FBT Seemed Successful for Early Intervention and Prevention of Anorexia
These two situations may have been cases of anorexia averted. Certainly, there is no evidence that either child was harmed in any way by the parents taking charge of meals for a limited time.

A common worry expressed by parents of children with early or mild symptoms of an eating disorder is that they do not want to take it more seriously than necessary. They worry that intervening aggressively early on may somehow make things worse, that over-pathologizing will build the child’s preoccupation, and that they will waste time and money. FBT, done in the context of the home with guidance by a therapist with FBT training, is less disruptive and relatively low cost, especially as compared to other eating disorder treatments. FBT may be particularly potent when initiated early in the disorder. Research indicates that our clinical experience supports that intervening earlier is much easier, faster, and cost-effective than treatments for well-established eating disorders.
At EDTLA, we believe these case studies illustrate the great potential that FBT offers for early intervention.
Get Early Intervention Support Through Family-Based Treatment (FBT) in Los Angeles, CA
When eating disorder symptoms first appear, taking action early can make a meaningful difference in recovery outcomes. Family-Based Treatment (FBT) is a well-researched approach that engages parents and caregivers from the start, helping restore nutrition, stabilize health, and reduce the risk of long-term complications.
You don’t have to wait or manage this process alone. Through FBT, families receive clear guidance, education, and ongoing support to address eating disorder behaviors while strengthening recovery at home. At Eating Disorder Therapy LA, our Los Angeles–based therapists specialize in early intervention for adolescents with anorexia, bulimia, and related eating disorders, and work closely with families to create a strong foundation for lasting recovery. Getting started is simple:
- Contact Eating Disorder Therapy LA to discuss early concerns and treatment options
- Complete our Google form so we can match your family with a compassionate FBT therapist in Los Angeles
- Begin supporting your teen with timely, evidence-based care
Other Services EDTLA Offers in Los Angeles, CA
Recognizing eating disorder symptoms early and responding with the right support can significantly improve recovery outcomes. Family-based treatment (FBT) equips caregivers with the tools and guidance needed to intervene quickly, restore health, and reduce the likelihood of the illness becoming more entrenched.
At Eating Disorder Therapy LA, we provide specialized, evidence-based care for individuals and families at every stage of life, including children, adolescents, college students, adults, and caregivers. Our trained therapists can treat the full range of eating disorders and related concerns. In addition to FBT, we offer treatment for Anorexia Nervosa, Atypical Anorexia, Bulimia Nervosa, Avoidant/Restrictive Food Intake Disorder (ARFID), and Binge Eating Disorder, as well as support for challenges such as excessive exercise, body image distress, and phobias related to swallowing, choking, or vomiting.
To ensure care is accessible and responsive, our Los Angeles-based practice offers both virtual therapy and eating disorder group therapy options. We also provide Small Group FBT and ARFID consultations, professional speaking engagements, school-based services, and clinical supervision for therapists seeking advanced expertise in eating disorder treatment.
For further education and support, we invite you to explore our Eating Disorder Blog and Dr. Muhlheim’s books, When Your Teen Has an Eating Disorder and The Weight-Inclusive CBT Workbook for Eating Disorders (available in 2026). To connect with our team, please call (323) 743-1122 or email Hello@EDTLA.com. We look forward to supporting early, effective, and lasting recovery.
About the Authors
Lauren Muhlheim
Dr. Lauren Muhlheim, Psy.D., FAED, CEDS-C, is the founder of Eating Disorder Therapy LA and a licensed psychologist with extensive experience treating eating disorders in children, adolescents, and adults. Her clinical expertise centers on evidence-based treatment for anorexia, bulimia, binge eating disorder, ARFID, and related concerns, with a strong emphasis on family-based treatment (FBT) for adolescents.
As one of the few FBT-certified therapists in Los Angeles, Dr. Muhlheim works closely with parents to support nutrition restoration, guide recovery at home, and help teens return to healthy development. She is the author of When Your Teen Has an Eating Disorder and The Weight-Inclusive CBT Workbook for Eating Disorders, and has created one of the only FBT training courses for dietitians. Licensed in California, Indiana, New York, and Oregon, with a Florida telehealth license, Dr. Muhlheim is widely recognized for her leadership in family-centered, weight-inclusive eating disorder care.
Therese Waterhous
Therese S. Waterhous PhD, RDN, CEDS-S, FAED is an eating disorder specialist in private practice in the Willamette Valley of Oregon. While no longer seeing patients, Therese remains active in teaching and training other healthcare professionals about eating disorders and advocating for those with eating disorders. As an advocate for those with eating disorders, Therese was one of the founding board members for the international non-profit advocacy group FEAST-ED (Families Empowered and Supporting Treatment for Eating Disorders). She delivers many local talks to various groups, educating them about eating disorders. In 2016-2017, she received and executed work on a grant from the local Coordinated Care Organization to train other healthcare professionals about eating disorder evaluation and treatment and extend eating disorder treatment to underserved Oregonians. She developed a state training for the Oregon Health Authority in 2021-2022 and is currently working on updating that training.
In the past, Therese served on the Oregon IAEDP (International Assn. for Eating Disorders Professionals) chapter board. Therese served on the Academy for Eating Disorders (AED) special interest group on Family-Based Treatment, the AED Medical Care Standards Committee and the AED Experts by Experience Committee. Currently, she serves AED on the Nutrition Task Force, the Clinical Standards of Care Committee, and the Special Interest Groups Oversight Committee.