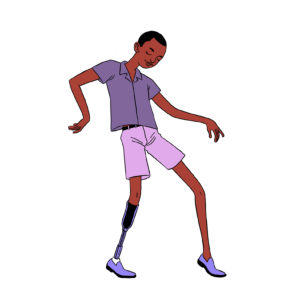
Despite being widely thought of as a disorder primarily affecting females, we know that people of all genders experience eating disorders. The experiences of males with eating disorders may be different so read on to learn more.
Prevalence rates
It is difficult to know exactly how many males are affected, partly because they have not been researched as much and partly because they are less likely to get diagnosed and treated.
Although it is widely quoted that only 10% of people with eating disorders are male, this is a likely underestimation. More likely, approximately 25% of individuals with anorexia nervosa and bulimia nervosa are male. Males make up even a larger percentage of the people with two more newly recognized diagnoses, Avoidant Restrictive Food Intake Disorder (ARFID) and Binge Eating Disorder. It is estimated that 40 percent of people with binge eating disorder are male. As many as 67 percent of children with ARFID may be male.
History
Eating disorders in males have been noted since 1689, when Richard Morton, an English physician, described 2 cases of “nervous consumption,” one in a male patient. Males later fell off the radar of eating disorders. Less than 1% of the papers on eating disorders focus on males.
Underrepresentation
Males have been largely excluded from the literature and research on eating disorders due to a variety of factors including stigma and biased assessment measures. Men may be less likely to endorse symptoms of what is commonly seen as a female illness and reluctant to ask for help. Because eating disorder awareness efforts typically target only girls, boys and men also may be less aware of eating disorders and less likely to recognize their problem as one. For these various reasons, males are likely underreported in prevalence statistics.
Additionally, since all of the available measures used to assess eating disorders were designed for females, they may not capture males with eating disorders. For example, the Eating Disorders Inventory has a question, ” I think my thighs are too large. ” This item is less likely to be endorsed by males because it does not reflect their body image concerns. A male-specific eating disorder assessment tool is the Eating Disorder Assessment for Males (EDAM). For example, a corresponding item on the EDAM might be something similar to, “I check my body several times a day for muscularity, ” which is more oriented toward males’ concerns.
Features
One of the most striking differences between males and females with eating disorders is the difference in body image concerns. This seems to be a reflection of the difference between perceived ideal female and male bodies. While women are encouraged to be thin, males are encouraged to be muscular. There is research indicating that while the ideal body shape for females has gotten thinner over the years, corresponding research shows the ideal for men has gotten bulkier and more muscular.
Whether an eating disorder presents as a desire for thinness or muscularity appears to be related primarily to gender role identification; that is, feminine self-identification appears to be a risk factor for the development in men of thinness-oriented eating disorder psychopathology, while masculine self-identification is linked with the drive for muscularity and may contribute toward the development in men of muscularity-oriented body image concerns.
There is a question as to whether muscle dysmorphia is a type of body dysmorphia (itself a type of obsessive-compulsive and related disorders) or an eating disorder. Dr. Stuart Murray’s research supports that it is an eating disorder because it typically includes both compulsive exercise practices and disordered eating. Disordered eating practices are usually central to muscle dysmorphia, which is why it is not just body dysmorphia. As with female eating disorders, the compulsive exercise practices associated with muscularity-oriented eating disorders are often driven by appearance rather than health or performance.
Muscularity disordered eating may look quite different than the disordered eating more commonly seen in females. Girls and women with eating disorders usually restrict intake of high calorie food items. Males with eating disorders may increase their intake, especially of protein sources, and may also use appearance-enhancing substances such as supplements, steroids, growth hormone, and clenbuterol.
Other Differences Between Male and Female Eating Disorders
Exercise is more central to male presentations of bulimia nervosa than is purging or laxative use. Male eating disorders most typically involve two dimensions for male body image: leanness and muscularity. These may often be mutually exclusive. This can cause a cyclical nature to male eating disorders of bulking (weight gain) followed by cutting (weight loss). Males with bulimia may also not engage in typical binge eating, but may instead have “cheat meals.”
Males with eating disorders have a later age of onset, a greater likelihood of previous overweight status, greater psychiatric comorbidity, and a greater risk for suicidality. They are also less likely to seek treatment and when they do, it is common after a longer period of illness, which reduces the likelihood of a full recovery. Males suffer from many of the same medical issues as females with eating disorders but also may experience decreased testosterone and problems with sexual functioning.
Treatment
Treatment for male patients with eating disorders must be gender-sensitive and address the stigma of being seen for what is commonly known as a female disorder. Clinicians should explore with male clients what it means for them to be male and how their body reflects that. Treatment with males often focuses more tightly on addressing exercise, which is often the first symptom to present and the last to remit.
Male Eating and Body Image Therapy Group
Learn more about EDTLA’s Eating and Body Image Therapy Group for Men ledy by Jonathan Dang, LMFT