TL;DR
At the 2018 International Conference on Eating Disorders, experts discussed the low BMI threshold (18.5) often used to define recovery from anorexia nervosa, suggesting it’s inadequate for many individuals, especially those with higher weights or atypical anorexia. Many parents and practitioners advocate for a more individualized approach to recovery weights, emphasizing that a higher target weight can lead to better mental health outcomes and fuller recovery. Research shows that many individuals do not achieve true recovery at lower BMIs, often requiring a weight restoration beyond standard guidelines. Family-Based Treatment (FBT) in Los Angeles focuses on personalized recovery strategies, engaging parents in the process for better outcomes. If you’re navigating these challenging conversations, expert support is available to help your teen achieve a healthy, realistic weight.
Defining Eating Disorder Recovery
Plenary on Defining Recovery
At the 2018 International Conference on Eating Disorders (ICED) in Chicago, I attended a plenary, Recovery from an Eating Disorder: How Do We Define It? What Does It Look Like? And Should It Always Be the Focus? During this plenary, Anna Bardone-Cone, Ph.D., spoke about the essential components of recovery from an eating disorder. She indicated that definitions of recovery should include the following three domains and proposed the following criteria for each domain of eating disorder recovery:
- Physical — defined as BMI greater than 18.5
- Behavioral— defined as the absence of any binge eating, vomiting, laxative use, or fasting within the past 3 months
- Cognitive — defined as EDE-Q subscales within 1 standard deviation of age-matched community norms.
Hold on a second—the weight criterion used to define recovery from anorexia nervosa in most studies is a BMI of only 18.5?
Response to the Plenary
Most in the full plenary room agreed that for anorexia nervosa recovery, a BMI of 18.5 is too low a criterion to declare all people recovered. I agree with Laura Collins Lyster-Mensh, who made the following tweets:
- Isn’t it possible that by setting target weights at the low end of the tail, we are holding patients in chronic mental illness?
- Setting low, population-based weight targets for ALL EATING DISORDERS means weight suppression and malnourishment and prevents psychiatric recovery for all but those who are genetically designed to be in smaller bodies, IMO.
I totally agree. If we now acknowledge that anorexia occurs in people of higher weights—a phenomenon often, and problematically, called “Atypical Anorexia”—then shouldn’t a BMI target as low as 18.5 be abandoned in favor of individualized recovery weights?
In fact, weight suppression researcher Michael Lowe was present at the plenary. During the Q&A, he proposed that rather than using a categorical definition of weight recovery (a single BMI number), we should use a continuum—for example, the recovered patient’s BMI relative to their pre-illness BMI.
How Are Recovery Weights Established in Research and Practice?
Unfortunately, there is very little consensus on how to determine whether a patient with a restrictive eating disorder is at a recovered or healthy weight. This affects research and practice. If researchers define recovery based on an 18.5 BMI, and this weight is really too low for many people with anorexia, what does this mean for the research studies? For one thing, in clinical trials, a lower percentage of people would be deemed “recovered,” showing our treatments to be even less successful than we believe them to be.
But it has bigger implications for the potential for patients to truly recover. If we set recovery weights higher, maybe more people will be treated to full recovery. Setting the BMI bar so low means we’re not insisting on full weight recovery for all people. As Laura Collins points out, the effect of this is that only those who are privileged enough to be in genetically smaller bodies may ever actually reach recovery.
And what are the ramifications for practitioners? There may not yet be an established way to determine a recovery weight. Consequently, many patients may never recover. If we acknowledge that gaining to a healthy body weight is a prerequisite for full psychological recovery, then we are dooming many people in larger bodies to a life of purgatory in which they remain insufficiently sick to need intensive treatment, but never achieve full recovery.
How Do Practitioners Set Recovery Weights?
In one recent paper, Jocelyn Lebow, Leslie A. Sim, and Erin C. Accurso surveyed 113 child and adolescent eating disorder treatment providers inquiring about the methods used to determine weight restoration in clinical practice. Their findings show:
- 40.7% of practitioners used growth curve data
- The remaining (nearly 60%) employed a diverse range of approaches
- Providers who specialize in Family-Based Treatment were significantly more likely to use an individualized approach to setting recovery weights, versus considering teen preference
Lebow and colleagues concluded that:
Although there is a modicum of endorsement for using growth curves to predict expected body weight, this is not universal practice and is inconsistent with methods used in treatment studies. The lack of an evidence-based method to calculate expected body weight—or even a best practice consensus for calculating this number—is a major oversight in the field that requires empirical attention.
Why Might Providers Set Recovery Weights Too Low?
What are some of the reasons providers might be setting recovery weights too low?
- No empirical consensus or guidelines on how to set the target weight
- Lack of available growth records data to determine an individualized recovery weight
- Financial limitations—insurance companies reduce costs by lowering treatment limits, which are facilitated by lower weight goals
- Client resistance—pushing for higher weights requires overcoming greater resistance and anxiety from the patient and sometimes the family over higher weights.
- Weight stigma—even treatment providers may be susceptible to society’s war on obesity, and consequently may err on the side of under-restoring a teen in recovery.
One Mother’s Response to the Plenary Tweets
On X, one mother responded to my conference tweets about an 18.5 BMI recovery goal as being too low and wrote the following:
- We need all professionals to understand the need for higher recovery weights. Recovery is about state not weight. So many parents know this, but are stuck with uneducated team members who undermine their work.
- If professionals consider a return to pre-eating disorder growth patterns for height and weight to be weight restoration, we parents are saying wrong. Eating disorder voices are very loud at this weight. We recommend an additional 10% for the first few years of recovery at least. This quiets the eating disorder voice, and patients are more likely to stay recovered.
- I want all current professionals worldwide to understand this. There are so many parents in our international group whose professionals are not getting it. Maybe it has not been studied officially, but anecdotally, we are seeing this in high numbers.
- If it’s not part of their training, providers should at least listen to and support parents in this. We are committed to our kids’ recovery every bit as much as they are.
- It takes parents a while to get it too. It’s frustrating for professionals when parents undermine. I was horrified at the first proposed recovery weight and was afraid of my child being made fat. But I got educated pretty quickly, opened my eyes, and realized I needed to take it further in order to achieve full recovery.
Helping Parents Get on Board With Higher Weights
Stephanie Zerwas, Ph.D. (not at the conference) chimed in on X and asked the parent:
- What language helped you as a parent to “get it? Parents often have a belief that being a little underweight can help their child not worry about weight gain, not realizing that it keeps kids stuck in limbo and hypervigilant.
The parent responded:
- What helped us parents “get it” was seeing those in our support group brave enough to take their kids to higher weights, reporting that their kids’ eating disorder voices finally quieted down. We keep repeating state, not weight = recovery and realized goal weights are set mostly too low
- Too many parents are upset that eating disorder professionals are saying their kids are recovered and not listening to them when they say their kids are still vulnerable, using behaviors, and need to be a higher weight. This is the power of parent groups. We know this needs to change.
- Parents also not understanding weight restoration is a moving target. They come to our group stating their child is weight restored and still struggling, and often clinging to a weight goal given years ago. There is no “Weight Restored” in eating disorder recovery, only “state restored.”
- We are seeing this extra 10% to be effective in many of our children who still struggle with eating disorder behaviors at 100% pre-illness percentile of growth. In the meantime, if patients are still struggling and parents want this, we should be supported. But yes, bring on the studies!!
What Do Parents Say About Recovery Weights?
As an FBT therapist in Los Angeles, I believe that parents do indeed know their children best and are an untapped resource to study this further. So, I took to X to ask parents to share their experiences about recovery weights being set too low. I got an overwhelming response. Below are some excerpts of what parents sent to me:
First Parent Response
At her lowest weight, our daughter was BMI of 21.9. Our doctor told us, “She is not at an anorexic weight.” She is currently BMI 31.6. We felt she was finally starting to shift her thinking when she was at around a BMI of 29.5.
Second Parent Response
When my daughter was 17, she lost 25 pounds. At her lowest, her BMI never fell below 20. Yet she was extremely ill. After she had regained about 14 pounds, her period returned, but her “state” was still awful. She is now in a range of BMI 25.5 to 26. The difference these last 5 pounds has made has been amazing. Her level of insight and flexibility is much higher. Amazingly, the higher her weight, the happier she is with herself and her body. Reflecting back, I am grateful that no one told us she was “recovered” when she got her period back. She needed to get and stay back up to the 80 to 85%ile as per her personal growth curve.
At the age of 19.75, she grew another .25 inch. If that isn’t proof she needed more weight, I don’t know what is! I hear so many stories in our group of parents being told to stop refeeding too early. Teams are generally not comfortable pushing weights back up to or above personal growth curves. We are lucky our team was an exception! In our online support group, we have seen time and time again that higher weights make a difference. And the extra weight generally comes with little risk.
Third Parent Response
My daughter was diagnosed at the age of 10.5 with anorexia. The original goal was to get my daughter from a BMI of 15.5 to a BMI of 18. In the next 2.5 years, my daughter needed 6000 calories a day and a very high-fat diet. She grew nearly 9 inches, went through full puberty, and doubled her initial body weight. Once her growth slowed and her metabolism went down and stabilized, we were able to get her weight up to around a BMI of 22, and that is when we saw TRUE RECOVERY begin. Eventually, she began to eat “extra.” She began to ask for things. She began to be able to eat independently.
Over the last 4 years, she has put on around 20 to 25 pounds on her own, naturally. Her BMI is now around 24 – 2,5 and she is in a 100% solid recovery. She eats intuitively, independently, and reports being free of the eating disorder voice. Fats, high calories, and a MUCH higher weight were essential to getting our daughter into recovery. If I had listened to the “experts,” I believe she would still be struggling.
 Fourth Parent Response
Fourth Parent Response
My daughter was 24.2 BMI at 13 years old when she started exercising excessively and then restricting. She lost a quarter of her body weight in 7 months, and our new pediatrician told her to gain 10 pounds and come back in 6 weeks. We fed her 6 times for a total of 4000 calories a day. She finally got her period at BMI 21.8, and within a few months, her anxiety was high, and the team suggested it was time to start exercising. My online support group spent a long time helping me understand my own fat phobia and really worked to help me set a higher target weight. My daughter grew another three inches. She is now BMI 23.5, and this is the healthiest I have ever seen her. If I had listened to the specialists, she would be just as sick as she was before.
Fifth Parent Response
At her lowest weight and her sickest, my daughter’s BMI was 19.3. We saw improvements in her state once she was over 25 BMI and in the “overweight” range. Had I allowed a reduction in her food intake at 23 BMI when it was suggested to me, my daughter would have been in a perpetual eating disorder purgatory.
Sixth Parent Response
My daughter’s current BMI is 24.6. Lower than that or increasing muscle over fat, it is as if her body goes into ‘starvation mode’ and she gets all silly and cranky, and her period is delayed.
Seventh Parent Response
My son was given a target BMI of 19 by his clinician. This was not from a growth chart; it was from a generic BMI chart. My son was still very unwell at that BMI. Thoughts were very strong, and the desire to restrict was high. He was living a half-life, tormented by anorexia. He was throwing away his lunch and manipulating the weight. His clinician was adamant that he did not need more weight and did not need more food, although I could see he was actually starving. She would not support me in taking his weight higher or increasing his meal plan. My online support group warned me that this was a common mistake with clinicians. I got my son (with great difficulty, after the clinician had insisted lower was okay) to a BMI of 24.
We have never looked back. We have our kid back. He is 16 years old, and he has been in a very strong recovery for some time now. I know the extra weight is what he needed to see recovery. He is living a normal teen life now, is happy, and fully functional. We are into year 3 now, and he still needs 3 meals and 2 snacks per day of at least 4000 calories to stay in recovery. We owe our son’s recovery to the wonderful advice from parents who had been in our situation before us. They knew from other parents before them that a generic BMI figure is not recovery. Recovery is a state and not a weight. It makes perfect sense, too. After all, we do not expect everybody to have the same shoe size.
Eighth Parent Response
My daughter was diagnosed approximately 18 months ago with Atypical Anorexia and was very unwell at a BMI of 19. I joined a support group just prior to her entering treatment. In large part due to the anecdotal advice and experience of others in the group, I was of the firm belief that we needed to weight restore my girl to her own individual weight, not to a particular BMI or any particular upper number.
Fortunately, our team was happy for me to take the lead with this approach, and we encouraged weight gain to wherever her behaviors began to abate, and her weight settled naturally on its own, with NO reduction in intake. This ended up being at a BMI of around 26, which I do not believe most clinicians would encourage. However, I truly do have my happy girl back, and I do not regret any one of those extra kilos. Her body has settled at a weight at which her mind is very well. I believe that if we had been given an upper number that she couldn’t go above, we would have trapped her in her anorexia needlessly for so much longer.
Ninth Parent Response
My daughter did not seem to actually begin true recovery until she was at 23.5 BMI. This was higher than the professionals in her life seemed comfortable with, but I proceeded with semi-confidence (having seen the results of higher weights in other patients, through their carers’ stories) and was never challenged. Before this higher BMI, she struggled so much with ED thoughts and behaviors – very little could get through to her…. therapy, talking, coaching, none were very helpful… only FOOD, in larger amounts that some professionals recommend (specifically with regards to fats – avocados, ghee/butter, olive oil).
At 23.5, something seemed to just “lift”. She began to be able to participate for herself. Though she still had many ED behaviors and thoughts, she could push them aside much of the time. She lost most of her body image issues, and began asking for food outside of the meal plan – especially things she used to enjoy (chocolate, etc.). Unbelievably, she began asking for MORE food. Consensus among carers in the groups seems to be that a 22-25 BMI is where most sufferers see true strides in recovery. It is very, very rare that a BMI under 22 is successful, at least when polled on the peer-to-peer carer support groups. Most often, it seems as though 23-24 is the “sweet spot” for many. My daughter has remained at this BMI (just shy of 24) for almost 6 months.
Summary of Recovery BMI
One online support group did their own survey: “At what BMI did you see real recovery?”
Here are the responses ( note that most were given a target bmi of 19 by their clinician, and had to fight against that, or had to walk away from their provider to get their child into recovery)
- BMI 21-22 4
- BMI 22 3
- BMI 22-23 4
- BMI 23 1
- BMI 23-34 5
- BMI 24 4
- BMI 24-25 4
- BMI 25 4
So out of 29 respondents, none got their kid into recovery at BMI 19 OR 20.
A Survey For Parents
I helped conduct a follow-up survey for parents, and I’m pleased to share that the first of our parent papers, Parents know best: Caregiver perspectives on eating disorder recovery. You can also read the press release about our parent study.
How We Set Recovery Weights at EDTLA in California
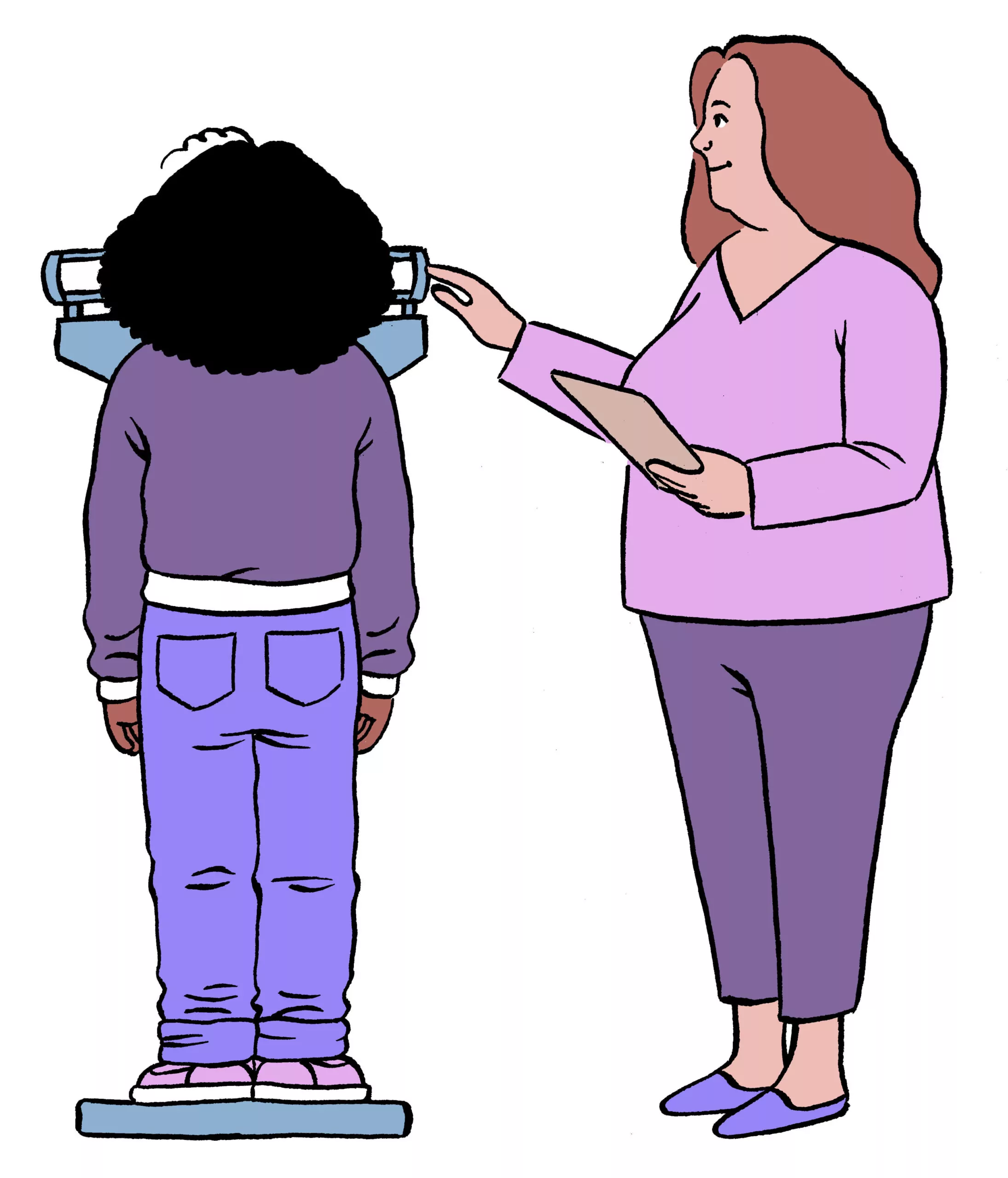
At our Los Angeles therapy practice, we use an individualized approach to setting recovery weights. Where the data is available, we review parental heights as well as the individual’s own growth records.
Get Expert Guidance on Recovery Weights Through Family-Based Treatment in Los Angeles, CA
When your child is struggling with an eating disorder, questions about weight restoration and recovery targets can feel confusing, and getting them wrong can delay healing. Family-based treatment (FBT) offers a research-backed approach that actively involves parents in supporting adequate weight restoration, improving medical stability, and laying the foundation for lasting recovery.
You don’t have to navigate these concerns on your own. Through FBT, families receive education, structure, and professional support to ensure recovery weights are set thoughtfully and adjusted as healing progresses. At Eating Disorder Therapy LA, our Los Angeles-based therapists specialize in family-based treatment for adolescents with anorexia, bulimia, and related eating disorders, helping families move forward with clarity and confidence. Getting started is simple:
- Reach out to Eating Disorder Therapy LA to discuss your concerns and next steps
- Complete our Google form so we can match your family with an experienced FBT therapist in Los Angeles
- Begin supporting your teen on a path toward full, sustainable recovery
Other Services With EDTLA in Los Angeles, California
Recovering from an eating disorder often requires more than willpower—it takes informed support, adequate weight restoration, and a treatment approach that addresses both medical and psychological healing. Family-based treatment (FBT) empowers caregivers to play a central role in recovery, helping restore physical health, normalize eating, and support long-term stability beyond the early stages of treatment.
At Eating Disorder Therapy LA, we offer specialized care for individuals and families at every stage of life, including children, adolescents, college students, adults, and caregivers. Our licensed therapists are trained in evidence-based treatments for the full range of eating disorders and related concerns. In addition to FBT, we provide therapy for Anorexia Nervosa, Atypical Anorexia, Bulimia Nervosa, Avoidant/Restrictive Food Intake Disorder (ARFID), and Binge Eating Disorder, along with support for excessive exercise, body image distress, and phobias related to swallowing, choking, or vomiting.
To ensure accessible and flexible care, our Los Angeles-based practice provides both virtual therapy and eating disorder group therapy options. We also offer Small Group FBT and ARFID consultations, professional speaking and training, school-based services, and clinical supervision for therapists seeking advanced expertise in eating disorder treatment.
For continued learning and support, we invite you to explore our eating disorder blog and Dr. Mulheim’s books, When Your Teen Has an Eating Disorder and The Weight-Inclusive CBT Workbook for Eating Disorders (available in 2026). If you’d like to connect with our team, please call (323) 743-1122 or email Hello@EDTLA.com. We look forward to supporting recovery that is thorough, sustainable, and guided by evidence.
About the Author
Dr. Lauren Muhlheim, Psy.D., FAED, CEDS-C, is the founder of Eating Disorder Therapy LA and a licensed psychologist in California, Indiana, New York, Oregon, and Florida. She has extensive experience treating various types of eating disorders, from onset to recovery. Her work focuses on evidence-based approaches to anorexia, bulimia, binge eating disorder, ARFID, and related concerns, with particular expertise in family-based treatment (FBT) for adolescents. As one of the few FBT-certified therapists in Los Angeles, Dr. Muhlheim helps parents take an active, informed role in weight restoration and recovery—an issue central to discussions about whether recovery weights are set too low. She is the author of When Your Teen Has an Eating Disorder and The Weight-Inclusive CBT Workbook for Eating Disorders, and has developed one of the only FBT training courses for dietitians, making her a recognized leader in weight-inclusive, family-centered eating disorder care.
Sources
Jocelyn Lebow, Leslie A. Sim & Erin C. Accurso (2017): Is there clinical consensus in defining weight restoration for adolescents with anorexia nervosa? Eating Disorders, DOI: 10.1080/10640266.2017.1388664