Exposure therapy is widely recognized as a necessary (and sometimes sufficient) ingredient of treatment for most of the anxiety disorders including phobias, panic disorder, and obsessive compulsive disorder. Anxiety is a core psychological feature of anorexia nervosa and bulimia nervosa. However, instead of being afraid of heights, speaking in public, having a heart attack, or contamination, individuals with eating disorders are primarily afraid of food, eating, and shape and weight.
Both cognitive-behavioral therapy and family based treatment, two empirically validated treatments for eating disorders, employ exposure techniques. Exposure works through the process of habituation, the natural neurologically-based tendency to get used to things to which you are exposed for a long time. During exposure, habituation occurs as people acclimate to their fear and come to realize that nothing actually dangerous is occurring. Habituation promotes new learning of safety, tolerance of fear feelings, and extinction of the fear avoidance urge.
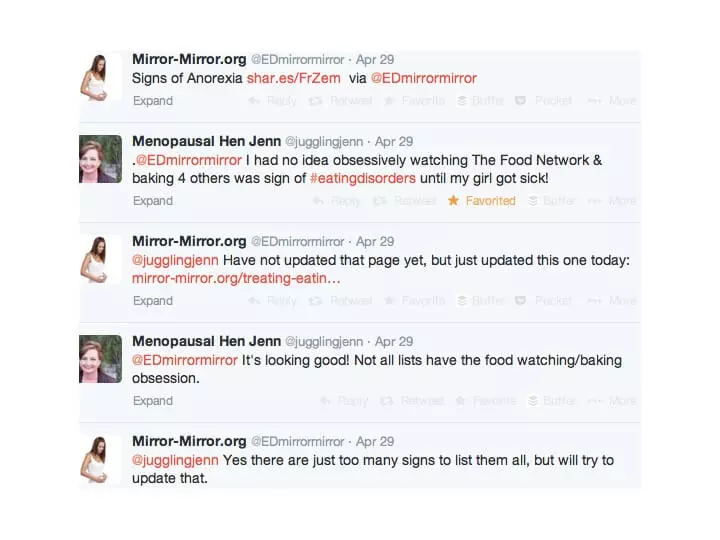
![family at family meal in FBT [Image description: a family with their backs to us sits around a table] Represents a potential family in California receiving FBT for their teens eating disorder](https://www.eatingdisordertherapyla.com/wp-content/uploads/2014/07/DALL·E-2023-12-01-19.14.32-a-family-is-seated-around-a-brown-conference-table.-There-are-2-parents-and-2-teenagers-sitting-and-their-backs-are-to-us.-Off-to-the-side-a-therapist5.png)