Meet Eating Disorder Therapy LA’s Prelicensed Associate Therapists
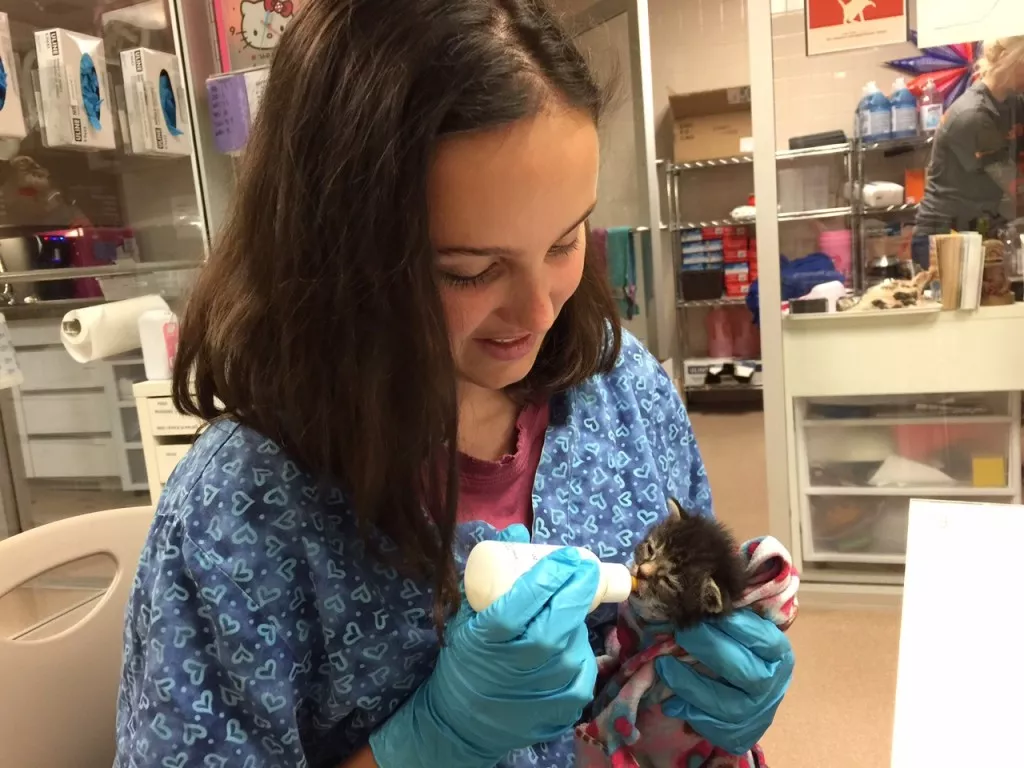
Eating Disorder Therapy LA provides training to prelicensed therapists (ACSW, AMFT, and APCC) in the Los Angeles area. Masters-level therapists work as employees while receiving extensive training in evidence-based therapy for eating disorders. Our clinical supervisor, Jonathan Dang, LMFT serves as primary supervisor of our prelicensed associate therapists. Mr. Dang is a certified eating disorder …
![The History of Eating Disorder Therapy LA [Image description: photos of 2 dark-haired women wearing t-shirts with Eating Disorder Therapy LA and the logo on the shirt; Dr. Carcieri is pregnant]](https://www.eatingdisordertherapyla.com/wp-content/uploads/2020/12/Lauren-and-Elisha.jpg)




![Starch- My Side of The Story- The Importance of Starch in Eating Disorder Recovery [Image description: drawing of a slice of bread with feet and a pirate hat and eye patch] Represents the misaligned food group](https://www.eatingdisordertherapyla.com/wp-content/uploads/2015/11/bread___n_butter_pirate_by_winter_artwork-d4qzhwq.jpg)