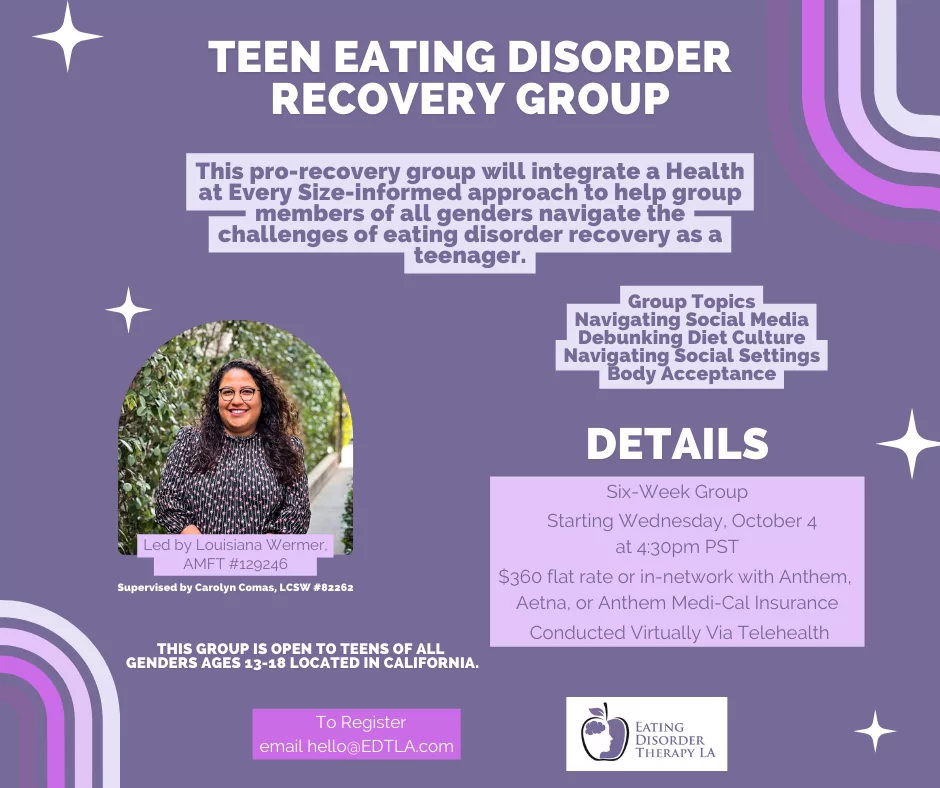
Teen Eating Disorder Recovery Group
As we have written elsewhere, we believe Family-Based Treatment (FBT) is a complete treatment for teens with eating disorders. Most teens will not need (or want) additional therapy. The one area where we think teens could use a little more support is in developing a strong anti-diet stance to stand up to weight stigma …
![Individual therapy in FBT [Image description: photo of a teen seated and facing an adult] Represents a potential teen client in therapy for an eating disorder in Los Angeles, California](https://www.eatingdisordertherapyla.com/wp-content/uploads/2022/01/priscilla-du-preez-F9DFuJoS9EU-unsplash.jpg)
![Externalizing your eating disorder in Los Angeles, California [Image description: a drawing of a girl facing a monster] Represents a potential teen with an eating disorder in Los Angeles, California externalizing her eating disorder](https://www.eatingdisordertherapyla.com/wp-content/uploads/2021/08/My-project1.png)
![Parenting During FBT [Image description: photo of one teen pushing another in a shopping cart] Represents a potential family with teens getting help for an eating disorder in Los Angeles, California](https://www.eatingdisordertherapyla.com/wp-content/uploads/2021/07/jakob-rosen-55MqyzQuZMI-unsplash-1.jpg)
![Supporting a Loved One with ARFID [Image description: woman looking disgusted at bowl of cereal] Represents a potential client with ARFID seeking treatment in Los Angeles, CA](https://www.eatingdisordertherapyla.com/wp-content/uploads/2021/03/rsz_1tamas-pap-xo5qtnr0a50-unsplash-1024x900.jpg)
![Easing Grief Through Connection (Coping Strategy for the Holidays) [Image description: jar of dimes]](https://www.eatingdisordertherapyla.com/wp-content/uploads/2020/12/dimes-smaller-1018x1024.jpg)
![How we set recovery weights [Image description: Drawing of a doctor weighing a teen patient] depicts potential person with an eating disorder receiving therapy in Los Angeles, California](https://www.eatingdisordertherapyla.com/wp-content/uploads/2020/10/scale-final1-876x1024.jpg)
![Structuring Your Eating Disorder Recovery Environment [Image description: hand visible writing in planner] represents a client in eating disorder recovery in Los Angeles, California writing a meal plan](https://www.eatingdisordertherapyla.com/wp-content/uploads/2020/10/stil-flRm0z3MEoA-unsplash-768x1024.jpg)
![College, COVID, and Eating Disorders [Image description: woman with mask in front of computer] represents a potential college student with an eating disorder having online therapy in California](https://www.eatingdisordertherapyla.com/wp-content/uploads/2020/08/engin-akyurt-WBM97UGM0QA-unsplash-scaled.jpg)